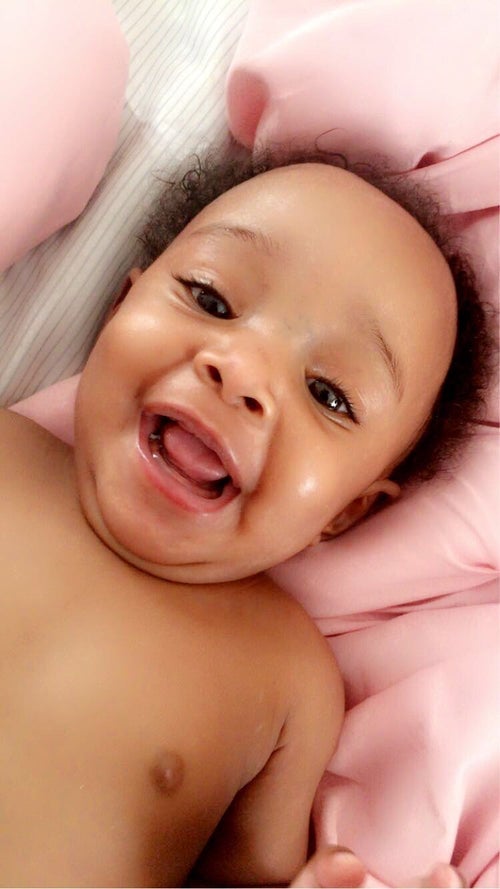
Sign up for Lani and others in need of a donor!

12,000,000
Donors registered with DKMS worldwide
110,000
Donations from our donors worldwide
Frequently asked questions
Who can register as a potential blood stem cell donor?
If you are between the ages of 18 and 55-years-old and in general good health, then you may be able to register as a blood stem cell donor.
If you have previously registered with DKMS or another donor center, there is no need to do so again, as you will already be available for searches worldwide. If you have been diagnosed with any chronic or serious illnesses (whether current or in the past), please check with us before signing up.
The National Marrow Donor Program has established medical guidelines that we follow to protect the safety of the donor. The following medical conditions would prevent a person from registering as a donor or from being cleared to donate.
- HIV
- History of heart surgery or heart disease
- Autoimmune disorders such as lupus, rheumatoid arthritis or multiple sclerosis
- Fibromyalgia
- Factor V
- Sleep apnea, breathing problems or severe asthma (daily inhalers are acceptable)
- Diabetes requiring insulin or injectable medication
- Hepatitis B or C
- Kidney or liver disease
- History of stroke, including TIA
- Multiple concussions or head injuries
- Chronic or severe neck or back problems
- Epilepsy or other seizure within one year
- History of blood clotting or bleeding disorders
- Personal history of cancer (exceptions: Stage 0 or in situ melanoma, breast, bladder, cervical and cured localized skin cancer such as basal cell or squamous cell carcinoma)
How are patients matched with donors?
A cheek cell sample is collected at registration. The sample is tested for the HLA characteristics and added to the global donor pool. Doctors can then search the registry and find a matching donor for their patient by comparing the patient's HLA to the donor's.
How does a bone marrow or blood stem cell donation work?
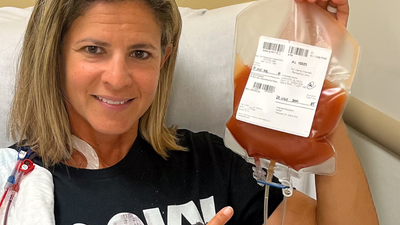
Peripheral stem cell donation
In about 80 percent of the cases the stem cells are taken from the bloodstream. The donor is administered the growth factor G-CSF for five days. This drug increases the number of stem cells in the peripheral blood, which are then obtained directly from the blood using a special procedure. The donation takes 4-8 hours on one or two consecutive days. No surgery is necessary, you can usually leave the clinic the same day. This procedure has been used at DKMS since 1996. During the administration of the drug, flu-like symptoms may occur. Long-term side effects are not known according to the current state of research.
Bone marrow donation
In this method, bone marrow is taken from the donor under general anaesthesia using a special syringe from the iliac crest. Two small incisions in the area of the rear pelvic bone are usually sufficient. The resulting wounds are so small that they only require a few stitches or often no stitches at all and heal quickly. The removal is performed in the prone position and takes about 60 minutes. With bone marrow donation, the risk is essentially limited to the anesthetic. About 5 percent of the bone marrow is taken from the iliac crest. Usually, the donor's bone marrow regenerates completely within 2 to 4 weeks. Local wound pain can occur, similar to a contusion. Only in rare cases can there be pain that lasts longer. The stay in the hospital lasts three days in total. In most cases, as a precautionary measure, a sick note is taken for a few days.
The type of withdrawal depends on the health condition of the patient. A donor should be prepared to use both methods.
What is blood cancer?
Blood cancer is the generic term for malignant diseases of the bone marrow or blood-forming system, in which normal blood formation is disturbed by the uncontrolled multiplication of malignant blood cells. Because of these cancer cells, the blood can no longer perform its vital tasks, such as fighting infections, transporting oxygen or stopping bleeding.
Curing blood cancer
Blood cancer patients can often only overcome the disease with the help of a stem cell donation from a suitable donor. In the case of leukemia and malignant lymphomas, the transfer of healthy stem cells is often the only chance of a cure.
Leukemia
A series of malignant diseases in which there is a pathologically increased proliferation of immature and therefore, non-functional white blood cells. Malignant lymphomas are divided into Hodgkin's disease (lymphogranulomatosis) and non-Hodgkin's lymphomas (lymphatic leukemia), according to their different characteristics.
Lymphoma, malignant
Malignant alteration of lymphatic tissue with swelling of the lymph nodes and pathological enlargement of the spleen. Malignant lymphomas are divided according to their different characteristics into Hodgkin's disease (lymphogranulomatosis) and non-Hodgkin's lymphomas (lymphatic leukemia), which originate from the lymph nodes.
What diseases do bone marrow and blood stem cells treat?
Bone marrow transplants can be the best or only treatment for patients fighting blood cancers like leukemia, lymphoma and myeloma, as well as approximately 70 other conditions including sickle cell disease, severe aplastic anemia, immune system disorders and inherited metabolic disorders. Nearly 20,000 Americans need bone marrow transplants every year (Source: U.S. Dept. of Health & Human Services based on data from NMDP).